Open Access, Peer-reviewed
eISSN 2093-9752

Open Access, Peer-reviewed
eISSN 2093-9752
Seung Tae Yang
Jung Woo Seo
Dae Hyeok Kim
Dong Won Kang
Jin Seung Choi
Gye Rae Tack
http://dx.doi.org/10.5103/KJSB.2016.26.4.391 Epub 2017 January 13
Abstract
Objective: This study aimed to evaluate and identify variables for the standing balance of elderly subjects with different balancing abilities by using Kinect and Wii Balance Board.
Method: The Berg Balance Scale (BBS) test was performed in 40 elderly subjects aged ≥65 years who can perform daily activities. The participants were divided into two groups, the healthy seniors (n = 20, BBS score ≥ 52) and the seniors with balancing problems (n = 20, BBS score < 52). Each group performed two standing tests (eyes open and eyes close) with two devices (Kinect and Wii Balance Board). The root mean square (RMS), mean distance (MDIST), range of distance (ROD), mean velocity, and 95% ellipse area were calculated from the measured data.
Results: Among the calculated variables, RMS, MDIST, and ROD in the mediolateral direction showed significant differences between the two groups and a negative correlation with BBS scores.
Conclusion: The results of the present study show that simple standing balance of the elderly can be measured with Kinect and Wii Balance Board, which are low-cost, easy to carry, and easy to use, by using the selected variables.
Keywords
Kinect sensor Wii Balance Board Standing balance Berg balance scale Elderly
Aging-induced deterioration of physical functions results in impaired balance, causing difficulties in daily living and increasing fall risks (Youm & Kim, 2012; Jeon, Park, Kang & Kim, 2009). Aging is closely related to postural sway, which is critical for maintaining balance, and many studies have been conducted on this topic (Woollacott & Shumway-Cook, 2002). Various studies performed measurements of standing body sway, which constitutes the basis of most daily living activities, as a means to assess individual balance, as these parameters present differ- rences between clinical populations in a noninvasive manner (Koslucher et al., 2012).
Traditionally, expensive specialized equipment such as force plates (Prado et al., 2007) or three-dimensional motion analyzers (McLoughlin, Barr, Crotty, Lord & Sturnieks, 2015) has been used for quantitative kinematic measurements of body sway, but more economic and user-friendly equipment such as Kinect Sensor (Microsoft, USA) and Wii Balance Board (WBB; Nintendo, Japan) has been gaining popularity in recent years. Depending on specific standing motions, Kinect provides a relatively accurate location of anatomical joint centers (AJC) by using depth sensors and red green blue (RGB) sensors, while WBB provides information on the center of pressure (COP). These two devices use different measurement methods, but share a common feature of ena- bling quantitative measurement of body sway without the need to attach separate sensors or markers on the subject's body. Furthermore, Kinect and WBB have been verified to parallel the traditional specialized equipment for use in clinical balance assessment using quantitative kinematic measurements (Clark et al., 2012; Clark et al., 2010).
However, previous studies that used Kinect and WBB suggested that these devices have positive effects as intervention tools for exercise games via their developed software (Vernadakis, Derri, Tsitskari & Antoniou, 2014; Goble, Cone & Fling., 2014), but their potential for use in clinical balance assessment of the elderly has hardly been docu- mented. In particular, Goble, Cone and Fling reported that WBB, with its low cost and portability, is a useful alternative to the traditional force platforms, but the balance metrics provided by the software are less effective in describing balance states (Goble et al., 2014). Therefore, parameters that are appropriate for clinical assessment of balance should be extracted by using Kinect and WBB, as doing so may add to the existing benefits of these devices (e.g., low cost and portability) and increase their value as assessment instruments by providing clinical meanings of balance assessment results.
In this context, in this study, we measured standing body sway by using Kinect and WBB in elderly subjects to verify the efficacy of these instruments in clinical balance assessment and to analyze the correlation between the parameters with significant intergroup differences and Berg Balance Scale (BBS) scores.
1. Participants
Forty elderly participants aged ≥65 years who were residing in a local community were recruited. The inclusion criteria were as follows: those capable of walking 10 meters without assistive devices and those with no visual impairment or lower motor neuron disease. The selected participants were assessed for any balance impairments by using the BBS. The BBS is comprised of 14 items in three categories (sitting, standing, and postural change), with 4 points for each item (total of 56 points). Based on the BBS scores, the participants were divided into the healthy older (HO) group (n = 20, BBS score ≥52) with independent daily living and normal balance, and impaired older (IO) group (n = 20, BBS score < 52) with impaired balance (Silsupadol et al., 2009).
Table 1 shows the physical characteristics and BBS scores in the two groups. The two groups only had a statistically significant difference in BBS scores (Table 1). All the participants learned the experiment method and provided informed consent prior to enrollment. This study adhered to the experimental protocol approved by the institutional review board of our institution.
|
Group |
Number of (n) |
Age (years) |
Weight (kg) |
Height (cm) |
BBS (score) |
|
HO |
20 |
75.05 ± 5.27 |
59.34 ± 9.16 |
152.91 ± 8.38 |
53.55 ± 1.05** |
|
IO |
20 |
76.60 ± 4.73 |
57.16 ± 7.46 |
150.56 ± 9.04 |
50.20 ± 1.28** |
2. Measurements
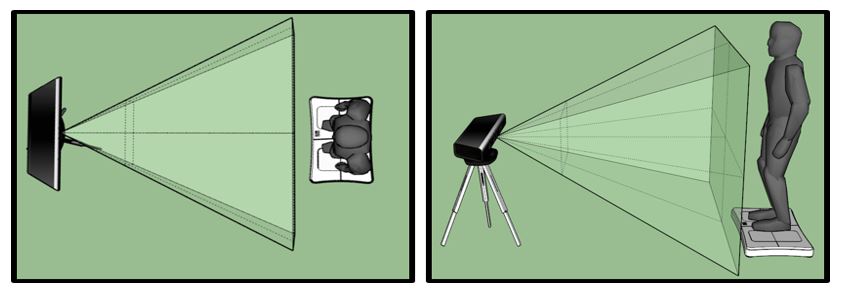
To assess standing balance, we performed two tests, one with eyes open (EO) and one with eyes closed (EC). The participants maintained their standing position for 30 seconds for each test (Costa et al., 2007) and were given sufficient time to rest in comfortable postures in be- tween tests. Kinect and WBB were synced to measure body sway while standing. Kinect was placed 2.5 meters in front of the participants, and WBB was placed underneath the participants' feet. As shown in Figure 1, the equipment was set such that the participants' bodies were within its angle of view, with the participants standing with their feet shoulder-width apart. While the participants maintained their standing posture, three-dimensional skeleton data, which show anatomical joint centers, were collected by using Kinect, and movement of the vertical COP trajectory was measured by using WBB. Kinect and WBB data were obtained simultaneously via MATLAB (MathWorks, USA) at a sampling frequency of 30 Hz.
3. Data processing
Kinematic parameters of body sway were extracted from the obtained data for a quantitative assessment of standing postures. The hip center data from Kinect and the COP trajectory data from WBB were used to calculate the kinematic parameters. We chose to use hip center data, as hip center data measured with Kinect have been reported to have a high correlation with those produced by a three-dimensional motion analyzer (r > 0.93) (Clark et al., 2012) and are the skeleton data closest to the center of mass (COM).
The high-frequency components of the anteroposterior (AP) and mediolateral (ML) body sway measurements obtained from Kinect and WBB (hip center, COP) were removed by using a 5-Hz low-pass filter. This study used root mean square (RMS), mean velocity (MVELO), mean distance (MDIST), and range of distance (ROD) as kinematic parameters used for the assessment of standing postures, all of which were meas- ured in the AP, ML, and resultant (Res) directions. Furthermore, we calculated the 95% ellipse area (AREA) in AP and ML directions in two dimensions. MATLAB (MathWorks, USA) was used for all data acquisition and processing.
4. Statistical analysis
The extracted parameters were tested for normality and analyzed with independent t tests and Mann-Whitney U test. BSS scores (clinical results) and Pearson's correlation coefficients were drawn by using SPSS 23.0 (IBM, USA) to examine the parameters that significantly vary between the groups. The level of significance was set as .05 for all the statistics.
Table 2 shows the standing parameters measured from two tests by using Kinect and WBB. The two groups showed significant differences in all the parameters collected with Kinect and WBB in the ML direction for both standing tests. In the AP direction, the two groups only showed significant differences in RMS, MDIST, and ROD with eyes close and MVELO with eyes open and eyes close. Of note, no significant inter- group differences were found in all the AP parameter values collected from Kinect. In general, the values of the parameters that showed significant intergroup differences were higher in the IO group than in the HO group. MVELO in all directions (AP, ML, Res) collected from WBB were significantly different between the two groups regardless of the standing condition (eyes open or eyes closed). The ROD, MVELO, and AREA that were measured with WBB were higher than those measured with Kinect (Table 2).
|
|
Variable |
Axis |
EO |
EC |
p Value |
|||
|
HO |
IO |
HO |
IO |
EO |
EC |
|||
|
Kinect |
RMS (mm) |
ML |
2.61 ± 1.17 |
4.28 ± 2.44 |
2.37 ±1.36 |
4.19 ± 2.58 |
* |
** |
|
AP |
4.07 ± 1.17 |
4.54 ± 1.58 |
4.70 ± 2.07 |
5.53 ± 2.13 |
|
|
||
|
Res |
4.91 ± 1.40 |
6.40 ± 2.52 |
5.43 ± 2.08 |
7.16 ± 2.81 |
* |
* |
||
|
MDIST (mm) |
ML |
2.10 ± 0.93 |
3.45 ± 1.91 |
1.94 ± 1.18 |
3.33 ± 2.06 |
** |
* |
|
|
AP |
3.35 ± 1.03 |
3.67 ± 1.29 |
3.82 ± 1.76 |
4.52 ± 1.85 |
|
|
||
|
Res |
4.31 ± 1.30 |
5.62 ± 2.24 |
4.73 ± 1.83 |
6.27 ± 2.54 |
* |
* |
||
|
ROD (mm) |
ML |
12.18 ± 6.49 |
19.89 ± 13.45 |
10.74 ± 5.95 |
18.89 ± 11.27 |
* |
** |
|
|
AP |
17.59 ± 4.68 |
20.61 ± 7.47 |
20.34 ± 8.65 |
23.58 ± 8.38 |
|
|
||
|
Res |
21.84 ± 6.63 |
29.42 ± 13.76 |
23.58 ± 9.04 |
30.92 ± 12.31 |
* |
* |
||
|
MVELO (mm/s) |
ML |
3.50 ± 2.14 |
6.12 ± 7.10 |
2.92 ± 2.32 |
4.76 ± 3.60 |
* |
* |
|
|
AP |
3.76 ± 1.55 |
4.72 ± 2.44 |
3.82 ± 1.97 |
5.40 ± 3.46 |
|
|
||
|
Res |
5.73 ± 2.73 |
8.64 ± 7.71 |
5.35 ± 3.26 |
7.99 ± 5.42 |
|
* |
||
|
AREA (mm²) |
2D |
197.21 ± 120.77 |
378.94 ± 349.70 |
198.58 ± 170.27 |
450.29 ± 481.94 |
* |
* |
|
|
WBB |
RMS (mm) |
ML |
2.50 ± 1.08 |
4.41 ± 2.45 |
2.39 ± 1.22 |
4.19 ± 2.69 |
** |
* |
|
AP |
4.55 ± 1.17 |
5.38 ± 1.76 |
5.25 ± 1.56 |
6.47 ± 2.05 |
|
* |
||
|
Res |
5.24 ± 1.40 |
7.09 ± 2.66 |
5.85 ± 1.72 |
7.89 ± 2.89 |
* |
* |
||
|
MDIST (mm) |
ML |
1.96 ± 0.82 |
3.55 ± 1.95 |
1.93 ± 0.99 |
3.28 ± 2.07 |
** |
* |
|
|
AP |
3.62 ± 0.99 |
4.31 ± 1.43 |
4.21 ± 1.21 |
5.14 ± 1.59 |
|
* |
||
|
Res |
4.48 ± 1.22 |
6.23 ± 2.40 |
5.02 ± 1.46 |
6.77 ± 2.50 |
** |
* |
||
|
ROD (mm) |
ML |
13.89 ± 6.94 |
22.27 ± 12.65 |
12.23 ± 6.33 |
22.03 ± 14.21 |
* |
** |
|
|
AP |
23.62 ± 6.29 |
28.63 ± 9.26 |
27.37 ± 8.71 |
34.40 ± 10.93 |
|
* |
||
|
Res |
27.81 ± 8.00 |
36.97 ± 13.87 |
30.37 ± 9.56 |
41.82 ± 15.37 |
* |
* |
||
|
MVELO (mm/s) |
ML |
4.99 ± 1.95 |
6.64 ± 2.61 |
5.58 ± 2.53 |
7.95 ± 3.76 |
* |
** |
|
|
AP |
10.63 ± 3.67 |
14.14 ± 5.39 |
14.71 ± 7.05 |
19.96 ± 7.51 |
* |
** |
||
|
Res |
12.65 ± 4.36 |
16.92 ± 6.10 |
16.74 ± 7.77 |
23.01 ± 8.81 |
** |
** |
||
|
AREA (mm²) |
2D |
217.22 ± 135.02 |
484.41 ± 437.07 |
244.61 ± 183.21 |
551.24 ± 509.48 |
* |
** |
|
Table 3 shows the correlation between the parameters extracted from the two types of equipment (Kinect and WBB) and BSS scores. The significance of the negative correlation between BBS score and all para- meters collected from Kinect and WBB were stronger in the ML direction than in the AP direction. All eyes-open parameters from WBB were significantly negatively correlated with BBS scores. RMS, MDIST, and ROD in the ML direction were significantly negatively correlated with BBS scores regardless of the measurement device and standing con- dition (Table 3).
|
Posture state |
RMS |
MDIST |
ROD |
MVELO |
AREA |
|||||||||
|
ML |
AP |
Res |
ML |
AP |
Res |
ML |
AP |
Res |
ML |
AP |
Res |
2D |
||
|
Kinect |
EO |
-.580** |
-.323* |
-.526** |
-.600** |
-.303 |
-.541** |
-.485** |
-.377* |
-.471** |
-.257 |
-.341* |
-.283 |
-.486** |
|
EC |
-.440** |
-.044 |
-.232 |
-.411** |
-.029 |
-.225 |
-.458** |
-.093 |
-.278 |
-.267 |
-.288 |
-.280 |
-.291 |
|
|
WBB |
EO |
-.616** |
-.429** |
-.574** |
-.630** |
-.427** |
-.590** |
-.581** |
-.459** |
-.563** |
-.517** |
-.396* |
-.448** |
-.528** |
|
EC |
-.459** |
-.290 |
-.393* |
-.457** |
-.281 |
-.397* |
-.444** |
-.336* |
-.413** |
-.370* |
-.334* |
-.354* |
-.393* |
|
In essence, RMS, MDIST, and ROD in the ML direction significantly varied between the elderly groups according to balance abilities and were significantly correlated with the traditional clinical assessment results (BBS scores). Thus, these parameters are determined to be adequate for use in clinical assessments of balance.
This study used Kinect Sensor and Wii Balance Board to quantify body sway in elderly subjects to extract parameters that significantly vary according to balance abilities. Furthermore, the correlation between the extracted parameters and the BBS scores, which is a traditional clinical balance assessment instrument, was examined.
Body sway in the ML direction is more important than that in the AP direction in the determination of elderly balance ability. After per- forming balance training in the elderly, Nagy et al. (2007) found that ML movement was considerably more improved than AP movement was and suggested that ML movement is more important in maintaining balance in the elderly. In our findings, the ML parameters extracted from Kinect and WBB significantly varied between the two elderly groups of normal and impaired balance, but all the AP parameters from Kinect did not significantly differ between the groups. From a kinematic perspective, the extracted AP parameters may be explained through the inverted pendulum motion about the ankle (Winter, Patla, Prince, Ishac & Gielo-Perczak, 1998). Reduced muscle activation caused by aging makes it difficult for the elderly to control ankle movement, causing more increased movement in the AP direction than in the ML direction. As reported in previous studies, we found that AP parameters had higher mean values than ML parameters. Just as elderly groups with different balance ability generally show similar trends of excessive AP sway, the AP parameters extracted from Kinect did not significantly differ between the two groups in this study.
All the parameters measured during standing using Kinect and WBB (RMS, MDIST, ROD, MVELO, and AREA) have also been documented in the literature to vary depending on differences in balance. In a study that examined young adults and the elderly to investigate differences in balance according to aging, Prieto et al. (1996) showed that body sway parameters (RMS, MDIST, ROD, MVELO, and AREA) well reflected the differences between the groups. In a similar study surveying standing body sway, Maranesi et al. (2016) also found significant differences in the same parameters among three groups according to fall experience (no fall, two or fewer falls, and multiple falls). In addition, Raymakers, Samson and Verhaar (2005) reported statistically significant intergroup differences (younger adults, healthy elderly, Parkinson's disease patients, and geriatric patients) in the parameters that describe the stability of standing sway (ROD, MVELO, and AREA) according to balance impair- ment. Similarly, we found statistically significant intergroup differences in the same parameters in this study. In particular, the MVELOs in all directions (ML, AP, and Res) obtained from WBB were significantly different between the two groups according to balance ability.
In general, the parameters with significant intergroup differences were higher in the IO group than in the HO group. Horak, Nutt and Nashner (1992) suggested that increased body sway indicates increased postural instability and that such trend is also common in patients with postural instability, such as those with Parkinson's disease. In addition, Prieto et al. (1996) also found that the group of elderly with relatively lower balance abilities had higher mean values of the parameters than the younger adults group.
Past studies used both three-dimensional motion analyzers and force platforms to simultaneously measure standing body sway to identify the features of movements of COM and COP. In Winter's (1995) study, COP sway in standing had a wider ROD, higher frequency, and higher amplitude than COM sway in standing. A similar trend was present in the data obtained from Kinect and WBB, which are low-cost devices, where the values of ROD and MVELO obtained with WBB were higher than those obtained with Kinect.
The parameters that were found to significantly vary according to the elderly's balance were further investigated to determine their adequacy as balance assessment parameters by examining their correlations with scores in the BBS, a traditional clinical assessment scale. In a previous study on standing postures of stroke patients, using COP trajectories, a strong negative correlation was found between the MVELO of COP and the BBS scores (Karlsson & Frykberg, 2000). Similarly, in a study that examined the correlation between sex-specific standing parameters by using COP in the elderly, Nguyen et al. (2012) reported that MDIST, RMS, MVELO, and AREA were negatively correlated with BBS scores regardless of sex. Furthermore, Allin, Beach, Mitz and Mihailidis (2008) reported a negative correlation between head sway in standing in the elderly and BBS scores. In our study, parameters extracted from Kinect and WBB were negatively correlated with BBS scores. All the parameters obtained with WBB with eyes open had significant negative correlations with the BBS scores. Based on the significant negative correlations be- tween the parameters extracted from Kinect and WBB with the trad- itional clinical balance assessment instrument (BBS scores), which are similar to previous findings, we can assert that increased body sway undermines balance by increasing postural instability (Lee et al., 2009).
The RMS, MDIST, and ROD in the ML direction were negatively cor- related with BBS scores, regardless of standing condition and meas- urement device (Kinect or WBB), and significantly varied between the two elderly groups of normal and impaired balance. Thus, we speculate that the RMS, MDIST, and ROD in the ML direction are key parameters in standing balance assessment using Kinect and WBB, devices that feature low-cost, simplicity, and portability, for the elderly.
This study used Kinect and WBB, which are portable and user-friendly devices, for quantitative measurements of standing postures of two elderly groups of normal and impaired balance. Based on our findings, we determined that RMS, MDIST, and ROD in the ML direction, which varied between the two groups and had strong negative correlations with BBS scores, are adequate parameters for the quantitative assess- ment of standing balance of the elderly using Kinect and WBB.
References
1. Allin, S. J., Beach, C., Mitz, A. & Mihailidis, A. (2008, August). Video based analysis of standing balance in a community center. In 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (pp. 4531-4534).
Crossref
Google Scholar
2. Clark, R. A., Bryant, A. L., Pua, Y., McCrory, P., Bennell, K. & Hunt, M. (2010). Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait & Posture, 31(3), 307-310.
Crossref
Google Scholar
PubMed
3. Clark, R. A., Pua, Y. H., Fortin, K., Ritchie, C., Webster, K. E., Denehy, L. & Bryant, A. L. (2012). Validity of the Microsoft Kinect for assessment of postural control. Gait & Posture, 36(3), 372-377.
Crossref
Google Scholar
PubMed
4. Costa, M., Priplata, A. A., Lipsitz, L. A., Wu, Z., Huang, N. E., Goldberger, A. L. & Peng, C. K. (2007). Noise and poise: enhancement of pos- tural complexity in the elderly with a stochastic-resonance-based therapy. Europhysics Letters, 77(6), 68008.
Crossref
Google Scholar
5. Goble, D. J., Cone, B. L. & Fling, B. W. (2014). Using the Wii Fit as a tool for balance assessment and neurorehabilitation: the first half decade of “Wii-search”. Journal of Neuroengineering and Rehabilitation, 11(1), 1.
Crossref
Google Scholar
PubMed
6. Horak, F. B., Nutt, J. G. & Nashner, L. M. (1992). Postural inflexibility in parkinsonian subjects. Journal of the Neurological Sciences, 111(1), 46-58.
Crossref
Google Scholar
PubMed
7. Jeon, K. K., Park, K. D., Park, S. H., Kang, Y. S. & Kim D. G. (2009). Differ- ences in Angle of the Lower Extremities and Electromyography of Elderly Women Experienced a Fall. Korean Journal of Sport Bio- mechanics, 19(2), 245-255.
Crossref
Google Scholar
8. Karlsson, A. & Frykberg, G. (2000). Correlations between force plate measures for assessment of balance. Clinical Biomechanics, 15(5), 365-369.
Crossref
Google Scholar
PubMed
9. Koslucher, F., Wade, M. G., Nelson, B., Lim, K., Chen, F. C. & Stoffregen, T. A. (2012). Nintendo Wii Balance Board is sensitive to effects of visual tasks on standing sway in healthy elderly adults. Gait & Posture, 36(3), 605-608.
Crossref
Google Scholar
PubMed
10. Lee, K. S. & Kang, Y. T. (2009). Study of Correlation between BBS, SPPB, TUG and COP during Quiet Standing in Elderly Women. Korean Journal of Sport Biomechanics, 19(3), 529-538.
Crossref
Google Scholar
11. Maranesi, E., Merlo, A., Fioretti, S., Zemp, D. D., Campanini, I. & Quadri, P. (2016). A statistical approach to discriminate between non-fallers, rare fallers and frequent fallers in older adults based on posturo- graphic data. Clinical Biomechanics, 32, 8-13.
Crossref
Google Scholar
12. McLoughlin, J., Barr, C., Crotty, M., Lord, S. R. & Sturnieks, D. L. (2015). Association of postural sway with disability status and cerebellar dysfunction in people with multiple sclerosis: a preliminary study. International Journal of MS Care, 17(3), 146-151.
Crossref
Google Scholar
13. Nagy, E., Feher-Kiss, A., Barnai, M., Domján-Preszner, A., Angyan, L. & Horvath, G. (2007). Postural control in elderly subjects participating in balance training. European Journal of Applied Physiology, 100(1), 97-104.
Crossref
Google Scholar
14. Nguyen, U. S. D., Kiel, D. P., Li, W., Galica, A. M., Kang, H. G., Casey, V. A. & Hannan, M. T. (2012). Correlations of clinical and laboratory measures of balance in older men and women. Arthritis Care & Research, 64(12), 1895-1902.
Crossref
Google Scholar
PubMed
15. Prado, J. M., Stoffregen, T. A. & Duarte, M. (2007). Postural sway during dual tasks in young and elderly adults. Gerontology, 53(5), 274-281.
Crossref
Google Scholar
PubMed
16. Prieto, T. E., Myklebust, J. B., Hoffmann, R. G., Lovett, E. G. & Myklebust, B. M. (1996). Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Transactions on Biomedical Engineering, 43(9), 956-966.
Crossref
Google Scholar
17. Raymakers, J. A., Samson, M. M. & Verhaar, H. J. J. (2005). The assess- ment of body sway and the choice of the stability parameter (s). Gait & Posture, 21(1), 48-58.
Crossref
Google Scholar
PubMed
18. Silsupadol, P., Shumway-Cook, A., Lugade, V., van Donkelaar, P., Chou, L. S., Mayr, U. & Woollacott, M. H. (2009). Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 90(3), 381-387.
Crossref
Google Scholar
19. Vernadakis, N., Derri, V., Tsitskari, E. & Antoniou, P. (2014). The effect of Xbox Kinect intervention on balance ability for previously injured young competitive male athletes: a preliminary study. Physical Therapy in Sport, 15(3), 148-155.
Crossref
Google Scholar
20. Winter, D. A. (1995). Human balance and posture control during standing and walking. Gait & Posture, 3(4), 193-214.
Crossref
Google Scholar
21. Winter, D. A., Patla, A. E., Prince, F., Ishac, M. & Gielo-Perczak, K. (1998). Stiffness control of balance in quiet standing. Journal of Neuro-physiology, 80(3), 1211-1221.
Crossref
Google Scholar
PubMed
22. Woollacott, M. & Shumway-Cook, A. (2002). Attention and the control of posture and gait: a review of an emerging area of research. Gait & Posture, 16(1), 1-14.
Crossref
Google Scholar
PubMed
23. Youm, C. H. & Kim, T. H. (2012). Effects of induced fatigue of ankle joint muscle on the capability and recovery of postural control during single-leg stance. Korean Journal of Sport Biomechanics, 22(2), 219-228.
Crossref
Google Scholar