Open Access, Peer-reviewed
eISSN 2093-9752

Open Access, Peer-reviewed
eISSN 2093-9752
Hyun Ju Kim
Su Young Jang
Petra Valouchova
Il Bong Park
http://dx.doi.org/10.5103/KJAB.2025.35.3.247 Epub 2025 October 21
Abstract
Objective: To investigate the effects of dynamic neuromuscular stabilization (DNS) on stair gait biomechanics in middle-aged women with chronic low back pain (CLBP).
Method: Eleven participants completed 10 weeks of DNS training. The center of pressure (COP), range of motion (ROM), ankle and hip joint moments, and Oswestry Disability Index (ODI) were assessed before and after the intervention.
Results: After Holm-Bonferroni correction, COP decreased in the anterior-posterior (AP) measures during ascent and in both AP and medio-lateral (ML) measures during descent (p < .05). During stair ascent, ankle ROM increased from 42.51° (IQR: 34.67-42.84) to 47.19° (IQR: 45.89-55.00) (p = .006), and during stair descent, ankle ROM decreased from 66.35° (IQR: 59.58-68.83) to 59.04° (IQR: 53.35-69.27) (p = .021). Additionally, during stair ascent, ankle plantarflexor moment improved from -0.04 (IQR: -0.11 to 0.32) to -0.36 (IQR: -0.45 to -0.31) Nm/kg (p = .003), and ODI scores significantly decreased from 12.45 ± 4.32 to 7.63 ± 3.67 (p = .001).
Conclusion: DNS training showed preliminary evidence of improvements in dynamic balance control, ankle range of motion, plantarflexor moment, and functional disability. These results suggest potential clinical relevance of DNS for stair gait rehabilitation, but larger randomized controlled trials are needed for confirmation.
Keywords
Dynamic neuromuscular stabilization Chronic low back pain Stair gait Center of pressure Joint moment Range of motion
Low back pain (LBP) is one of the most common musculo- skeletal disorders worldwide, with a reported lifetime pre- valence of approximately 80% (Violante, Mattioli & Bonfiglioli, 2015). Among these cases, chronic low back pain (CLBP) accounts for about 23% (Gibbs, McGahan, Ropper & Xu, 2023; Maher, Underwood & Buchbinder, 2017; Meucci, Fassa & Faria, 2015). CLBP is recognized as a multifactorial condition influenced by genetic, occupational, lifestyle, and psychosocial factors. It is also considered a major public health issue due to the substantial healthcare costs it imposes on society (Victora Ruas and Vieira, 2017; Vlaeyen et al., 2018).
Although most cases of CLBP are classified as non-specific, impaired neuromuscular control and failure of motor regulation under repetitive or compressive loading have been identified as key contributing mechanisms (Firouzabadi, Arjmand, Zhang, Pumberger & Schmidt, 2024; Kienbacher et al., 2016). In add- ition, reduced strength and lateral imbalance of the core and hip muscles, which play a critical role in spinal stability, are commonly observed in individuals with CLBP (de Sousa et al., 2019; Pizol, Miyamoto & Cabral, 2024; Stöwhas, Droppelmann, Jorquera & Feijoo, 2024). Patients with CLBP often exhibit not only altered motor control strategies but also deficits in core muscle function and proprioceptive impairments (Alshahrani, Reddy & Ravi, 2025; Sung, Abraham, Plastaras & Silfies, 2015). These physiological impairments can lead to reduced postural control during routine functional tasks such as walking or stair negotiation (Lima, Ferreira, Reis, Paes & Meziat-Filho, 2018; Poulsen and Cabell, 2024).
Stair ambulation is a high-level functional task that requires coordinated interaction between the trunk and lower limbs, involving core stability, lower limb joint alignment, and pro- prioceptive function (Kovacikova et al., 2020; Kuai et al., 2018; Tong et al., 2017). However, individuals with chronic low back pain often struggle to maintain an efficient gait pattern due to pain-related avoidance behavior and fear of movement. This typically results in reduced step length, limited joint range of motion, and increased postural sway (Castro-Méndez et al., 2021; Koch and Hänsel, 2018, 2019). Such alterations become more pronounced during complex functional tasks such as stair walking, and may lead to excessive compensatory move- ments of the lower limbs or abnormal distribution of joint moments (Chiu, Chang, Dennerlein & Xu, 2015; Wenzel, Hunt, Holcomb, Fitzpatrick & Brown, 2023).
Women differ from men in several physiological and func- tional characteristics, including hormonal fluctuations related to the menstrual cycle, anatomical structure, muscle strength, and neuromuscular control. These factors have been reported to impose greater strategic demands for maintaining postural stability during gait (Khowailed and Lee, 2021; Wohlgemuth et al., 2021). Therefore, in middle-aged women with CLBP, inefficiencies in lower limb joint angles, moment distribution, and balance control may be more pronounced.
Exercise interventions for women with CLBP have primarily focused on core stabilization, incorporating approaches such as Pilates, yoga, and proprioceptive training (Coulombe, Games, Neil & Eberman, 2017; Gorji, Mohammadi Nia Samakosh, Watt, Henrique Marchetti & Oliveira, 2022; Kofotolis, Kellis, Vlachopoulos, Gouitas & Theodorakis, 2016; Zahedi and Kiyani, 2020). However, most of these interventions have been per- formed under static conditions, and attempts to improve dynamic stability and inter-joint coordination during actual movement tasks remain limited.
Building upon this background, the present study seeks to apply DNS in middle-aged women to simultaneously promote trunk stability and functional coordination of the lower limb joints under dynamic conditions. Grounded in developmental kinesiology, DNS integrates the retraining of intra-abdominal pressure, postural alignment, breathing control, and muscle coordination, with a central focus on restoring movement strategies centered on the central nervous system (Frank, Kobesova & Kolar, 2013; Yoon and You, 2017). Unlike traditional static core stabilization exercises, DNS is distinguished by its ability to enhance coordination and postural control in dynamic, real-life conditions (Babagoltabar-Samakoush, Aminikhah & Bahiraei, 2025; Huang et al., 2025). Therefore, it is expected to positively influence postural regulation, inter-joint coordination, and the redistribution of joint moments even during complex functional tasks such as stair ambulation.
To date, studies examining the effects of DNS on COP con- trol, ROM and joint moment in the ankle and hip during stair gait in middle-aged women with chronic low back pain remain limited.
Accordingly, this pilot study aims to investigate the bio- mechanical effects of DNS by analyzing primary outcomes of COP parameters and sagittal plane ROM during stair ascent and descent before and after the intervention. In addition, joint moments of the lower limbs, walking speed, and the ODI, which reflects levels of pain and functional disability, were assessed as secondary outcomes to comprehensively examine the clinical applicability of DNS.
1. Participants
This study is involving 11 middle-aged women with non-specific chronic low back pain who had no regular exercise experience within the past six months and no limitations in performing daily activities. Recruitment was conducted through announcements on university bulletin boards at B University. Eligibility was confirmed through a brief screening interview addressing exercise history, pain characteristics, and daily activity limitations. All participants were informed about the study procedures and provided written consent. Participant adherence was high, with an attendance rate of -95%. No adverse events or analgesic use were reported.
Descriptive characteristics of the participants are presented in (Table 1).
|
Characteristics |
Age
(years) |
Height
(cm) |
Weight
(kg) |
BMI
(kg/m2) |
|
Average |
56.55±3.88 |
158.58±6.33 |
62.35±6.67 |
24.80±2.35 |
|
Note.
Values are presented as mean ± standard deviation |
||||
The specific inclusion criteria for the participants were as follows:
(1) having been diagnosed with chronic low back pain by a physician;
(2) experiencing non-specific chronic low back pain for more than three months;
(3) women aged between 40 and 64 years.
The specific exclusion criteria were as follows:
(1) individuals with acute intervertebral disc herniation;
(2) individuals who had undergone orthopedic surgery related to lumbar spine issues within the past six months;
(3) individuals with structural abnormalities in bones, nerves, or muscles (e.g., fractures or neurological/muscualr dis- orders);
(4) individuals with tissue damage or inflammatory conditions;
(5) individuals with cardiovascular disease;
(6) individuals currently undergoing psychiatric treatment or taking psychiatric medications.
2. Procedure
An exploratory pilot study was conducted in which a 10-week DNS exercise program was implemented twice a week following baseline assessments. All participants were informed of the study's purpose and procedures and provided written informed consent. Pre- and post-intervention comparisons were conducted with identical assessment tools and testing conditions.
Gait assessment was performed at each participant's self-selected speed using a staircase with a height of 18 cm for both ascent and descent tasks. Prior to data collection, partici- pants practiced the stair walking task to ensure familiarity with the procedure. Each participant performed five stair ascents and five stair descents, leading with the dominant leg, for a total of ten trials. Two force plates were embedded in the staircase, and data from the second step were used for analysis. A single stance phase, defined from heel-strike to toe-off, was extracted for each trial. An illustration of the staircase used for the task is provided in (Figure 1).

Marker trajectory data were collected at a sampling rate of 100 Hz using a six-camera infrared motion capture system (Vicon MX-T20, Oxford Metrics Ltd., Oxford, UK). Ground reaction force (GRF) and COP data were recorded at 1,000 Hz using an AMTI force platform (OR6, Watertown, MA, USA), and all data were synchronized with the Vicon system for integrated analysis.
Reflective markers for joint kinematic analysis were attached to key anatomical landmarks based on the Plug-in Gait lower-body model. Marker placement included the bilateral anterior superior iliac spines (ASIS), posterior superior iliac spines (PSIS), mid-thighs, patellae, mid-shanks, lateral malleoli, dorsum of the feet, and heels.
To ensure accurate marker tracking and minimize clothing interference, all participants wore tight-fitting shorts and per- formed the tasks barefoot (Perrin et al., 2023).
3. Data analysis
The primary outcome measures of this pilot study were COP parameters (range, velocity, and RMS in AP and ML directions) and ankle and hip ROM during stair ascent and descent. The secondary outcome measures were ankle and hip joint moments and gait speed during stair ascent, as well as the ODI.
1) Center of pressure analysis during stair ascent and descent
COP was analyzed based on displacement in the AP and ML directions. The primary variables included range, velocity, and RMS. COP coordinates were automatically calculated using Vicon Nexus software, based on ground reaction force and moment data collected at 1,000 Hz via a force platform. The stance phase was defined from heel-strike to toe-off. To minimize the influence of gait speed, COP velocity was nor- malized to stance duration. All COP variables were indepen- dently extracted for stair ascent and descent tasks.
2) Joint angle analysis during stair ascent and descent
The kinematic characteristics of the lower limb joints were analyzed by examining the sagittal plane joint angles of the ankle and hip. Joint angles were calculated using the Plug-in Gait model based on marker trajectory data. During the stance phase, the maximum flexion and maximum extension angles were extracted, and the difference between these two values was defined as ROM. The analysis was based on three gait cycles selected according to accurate foot placement identi- fication and signal quality. Each joint variable was extracted from Vicon Nexus, organized in Excel, and the average value was used for further analysis.
3) Joint moment analysis during stair ascent
Lower limb joint moments were analyzed in the sagittal plane for the ankle and hip joints using an inverse dynamics approach based on the Newton-Euler method. To evaluate the propulsion strategy, joint moment values were extracted at the toe-off phase, the end of the stance phase (McFadyen and Winter, 1988).
Joint moments were normalized to body weight (kg) and expressed in units of Nm/kg. GRF data were filtered using a fourth-order zero-lag Butterworth low-pass filter with a cutoff frequency of 10 Hz, commonly applied in stair-walking studies to reduce high-frequency noise while preserving signal in- tegrity (Crenna, Rossi & Berardengo, 2021; Steingrebe, Sell, Ehmann & Stein, 2025). Joint centers were automatically esti- mated using the Plug-in Gait lower-body model. Final joint moments were calculated based on segmental linear and angular kinematic data. According to the Plug-in Gait conven- tion, ankle plantarflexor moments were expressed as negative values and dorsiflexor moments as positive values, while hip flexor moments were defined as positive values and extensor moments as negative values. Therefore, during stair ascent at toe-off, the positive values observed at the hip reflect flexor moments, whereas the negative values at the ankle reflect plantarflexor moments.
4) Walking speed analysis during stair ascent
Walking speed during stair ascent was analyzed as a com- plementary secondary outcome, as joint moments are known to be highly sensitive to gait velocity (Buddhadev, Smiley & Martin, 2020; Goldberg & Stanhope, 2013). Spatiotemporal parameters, including gait speed, were automatically calculated in Vicon Nexus software based on marker trajectories and event detection (heel contact and toe-off).
5) Oswestry Disability Index assessment
In this study, ODI was used to assess the level of functional disability caused by low back pain. The ODI consists of 10 items, each evaluating the degree of limitation in daily activities such as personal care, walking, sitting, lifting, and social life.
4. Exercise intervention
The DNS exercise program was conducted twice per week for a total of 10 weeks, with each session lasting approximately 50 minutes. Each session consisted of a 10-minute warm-up, a 35-minute main exercise segment, and a 5-minute cool-down. All exercises were based on the principles of DNS, emphasizing postural alignment, intra-abdominal pressure control, and movement patterns derived from developmental kinesiology (Babagoltabar-Samakoush et al., 2025; Huang et al., 2025).
Exercises were performed on mats in a university gymna- sium, and intensity was gradually adjusted by increasing the number of repetitions over the 10-week period. Sessions were conducted in small groups and supervised by a certified trainer (15+ years' experience), who provided continuous pos- tural correction and verbal feedback to all participants. Exercise fidelity and adherence were ensured through direct supervision. No adverse events were reported during the intervention.
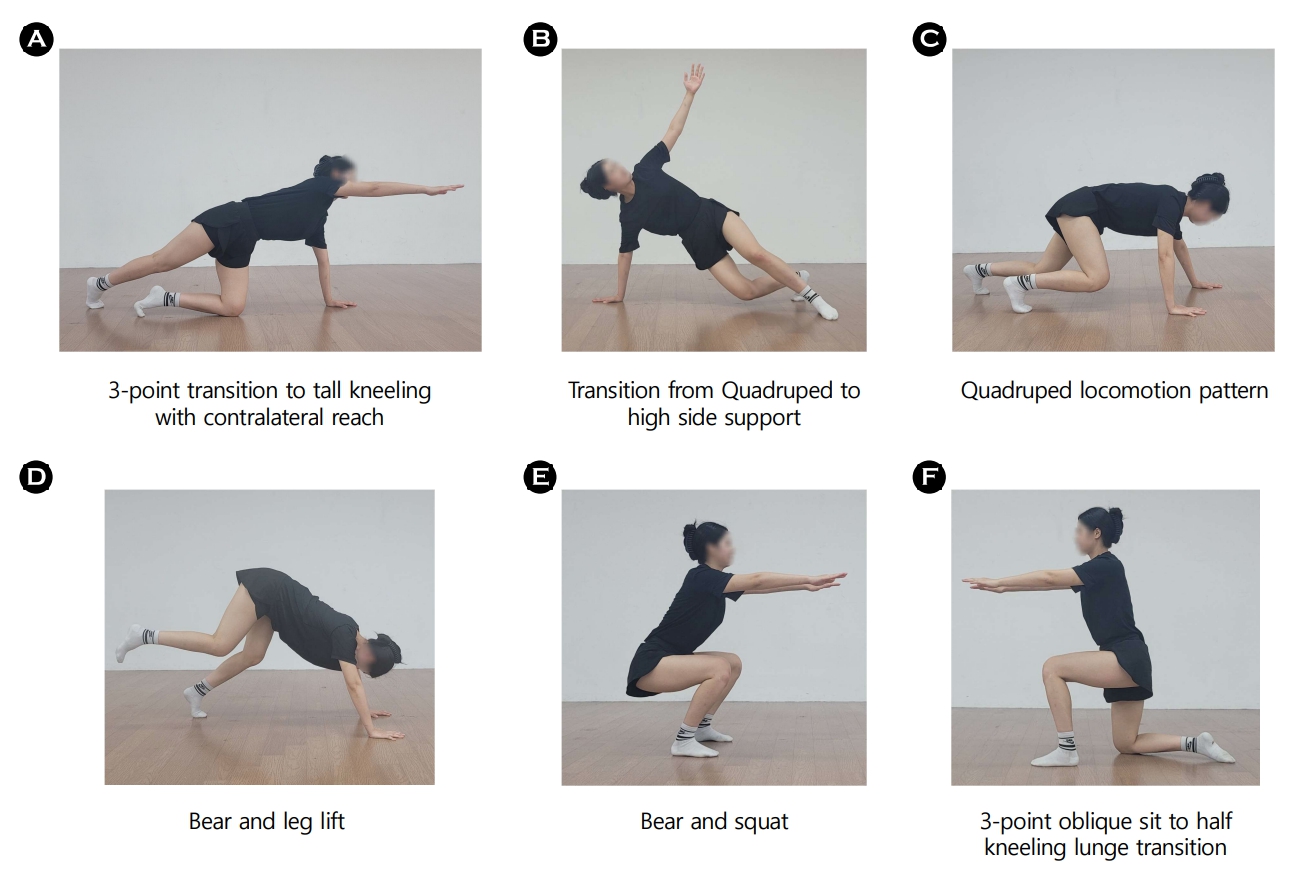
All exercises included in the program are described in (Table 2), and six representative DNS exercises are illustrated in (Figure 2).
|
Training |
10
weeks |
Time
/ Reps |
|
Warm-up |
1. Supine breathing |
10
/ 6 |
|
|
2. Supine cross-pattern activation |
|
|
DNS
exercise |
1.
Side-lying rolling |
35
/ 6-8 |
|
|
2.
Prone & quadruped rocking |
|
|
|
3.
Prone position with head and chest elevation |
|
|
|
4.
Contralatetal hip extension in quadruped |
|
|
|
5.
3-point transition to tall kneeling with contralateral reach |
|
|
|
6.
Quadruped locomotion pattern |
|
|
|
7.
Transition from Quadruped to high side support |
|
|
|
8.
Bear and leg lift |
|
|
|
9.
Bear and squat |
|
|
|
10.
3-point oblique sit to half kneeling lunge transition |
|
|
Cool-down |
1. Resting position for deep stabilization |
5
/ 6 |
|
|
2. Prone resting with diaphramatic control |
|
5. Statistical analysis
All data collected in this pilot study were analyzed using IBM SPSS Statistics, version 25.0 (IBM Corp., Armonk, NY, USA). Data normality was assessed using the Shapiro-Wilk test and Q-Q plots. Given the small sample size and violation of normality in most variables, non-parametric tests were primarily applied. Specifically, pre-post changes in ODI, which satisfied the normality assumption, were analyzed using a paired samples t-test, while all other outcomes (COP, ROM, joint moment, and walking speed) were analyzed using the Wilcoxon signed-rank test. Effect sizes were calculated (Cohen's d for parametric, r for non-parametric tests) and interpreted using Cohen's criteria. In addition, correlation analyses between ODI and biomechanical outcomes (COP parameters, and ROM) were conducted using Spearman's rank correlation coefficients.
Results are reported by predefined primary and secondary outcomes. Primary outcomes included COP parameters and ROM. COP outcomes were grouped into four families and corrected using the Holm-Bonferroni procedure (α = .05), whereas ROM outcomes were treated as predefined primary variables and analyzed independently. Secondary outcomes included joint moments, walking speed, and the ODI. In addition, correlation analyses were conducted between the primary outcomes and ODI. Detailed results for each outcome are summarized in (Tables 3-7).
|
Task |
Variables |
Pre (Median [IQR]) |
Post (Median [IQR]) |
z |
p |
r |
95% CI |
|
Stair |
AP-range (mm) |
37.3 [33.04, 46.50] |
26.86 [26.46, 29.34] |
-2.845 |
.004 |
0.86 |
4.88, 17.2 |
|
AP-velocity (mm/s) |
4.56 [4.28, 5.91] |
3.78 [3.18, 4.77] |
-2.756 |
.006 |
0.83 |
0.43, 1.64 |
|
|
AP-RMS (mm) |
1.15 [0.95, 1.58] |
1.10 [0.86, 1.35] |
-0.445 |
.657 |
0.13 |
-0.18, 0.39 |
|
|
ML-range (mm) |
9.92 [5.14, 13.73] |
7.19 [5.22, 9.26] |
-1.334 |
.182 |
0.40 |
-1.16, 5.54 |
|
|
ML-velocity (mm/s) |
2.05 [1.05, 2.19] |
1.74 [1.11, 1.87] |
-1.423 |
.286 |
0.43 |
-0.18, 0.68 |
|
|
ML-RMS (mm) |
4.30 [3.68, 4.73] |
3.77 [3.00, 4.35] |
-2.312 |
.021 |
0.70 |
0.15, 0.78 |
|
|
Stair |
AP-range (mm) |
38.50 [32.61, 45.17] |
31.68 [26.68, 35.00] |
-2.667 |
.008 |
0.80 |
1.74, 14.7 |
|
AP-velocity (mm/s) |
5.86 [5.00, 7.21] |
5.16 [4.49, 5.68] |
-2.401 |
.016 |
0.72 |
0.18, 2.47 |
|
|
AP-RMS (mm) |
1.41 [1.13, 1.87] |
1.39 [1.16, 1.61] |
-1.423 |
.155 |
0.43 |
-0.09, 0.39 |
|
|
ML-range (mm) |
13.74 [7.14, 17.38] |
9.41 [7.80, 15.15] |
-2.667 |
.008 |
0.80 |
1.07, 3.96 |
|
|
ML-velocity (mm/s) |
2.47 [1.56, 3.39] |
2.46 [1.53, 3.17] |
-2.134 |
.033 |
0.64 |
0.01, 0.63 |
|
|
ML-RMS (mm) |
4.41 [3.84, 4.88] |
4.05 [3.36, 4.25] |
-2.934 |
.003 |
0.88 |
0.25, 0.68 |
|
|
Note.
Values are median (interquartile range) p-values
are from Wilcoxon signed-rank test (pre vs. post) r =
effect size (small = 0.1, medium = 0.3, large ≥ 0.5) AP
= anterior-posterior; ML = medial-lateral 95%
CI = bias-corrected and accelerated (BCa) bootstrap confidence interval for
the median difference |
|||||||
|
Task |
Variables |
Pre (median [IQR]) |
Post (median [IQR]) |
z |
p |
r |
95% CI |
|
Stair |
Ankle ROM (°) |
42.51 [34.67, 42.84] |
47.19 [45.89, 55.00] |
-2.756 |
.006 |
0.83 |
-14.70, -2.51 |
|
Hip ROM (°) |
63.97 [62.37, 65.31] |
60.76 [52.60, 68.27] |
-1.334 |
.182 |
0.40 |
-3.24,
10.10 |
|
|
Ankle moment (Nm/kg) |
-0.04
[-0.11, 0.32) |
-0.36
[-0.45, -0.31] |
-2.934 |
.003 |
0.88 |
0.26, 2.90 |
|
|
Hip momet (Nm/kg) |
0.74
[-0.54, 1.63] |
1.12
[-2.47,2.13] |
-0.889 |
.374 |
0.27 |
-1.42, 22.60 |
|
|
Walking speed (m/s) |
0.42
[0.40, 0.48] |
0.46
[0.41, 0.50] |
-1.078 |
.281 |
0.34 |
-0.05, 0.02 |
|
|
Stair |
Ankle ROM (°) |
66.35 [59.58, 68.83] |
59.04 [53.35, 69.27] |
-2.312 |
.021 |
0.70 |
0.98, 12.00 |
|
Hip ROM (°) |
15.88 [13.36, 17.16] |
16.35 [15.48,
20.51] |
-1.600 |
.110 |
0.48 |
-4.34, 0.70 |
|
|
Note. Values are median (interquartile range) p-values are from Wilcoxon signed-rank test (pre
vs. post) r = effect size (small = 0.1, medium = 0.3, large
≥ 0.5) 95% CI = bias-corrected and accelerated (BCa)
bootstrap confidence interval for the median difference |
|||||||
|
Variable |
Pre |
Post |
t |
p |
d |
95% CI |
|
Total ODI score |
12.45±4.32 |
7.63±3.67 |
6.544 |
.001 |
1.97 |
3.18, 6.46 |
|
Note. Values are presented as mean ± standard deviation p-values
are from paired samples t-test (pre
vs. post) Cohen's d indicates effect size for paired t-test (small = 0.2, medium = 0.5,
large = 0.8) |
||||||
|
Variables |
p
(Spearman) |
p |
|
AP-range (mm) |
-0.189 |
.579 |
|
AP-velocity (mm/s) |
0.345 |
.299 |
|
AP-RMS (mm) |
0.083 |
.809 |
|
ML-range (mm) |
-0.184 |
.588 |
|
ML-velocity (mm/s) |
-0.354 |
.285 |
|
ML-RMS (mm) |
-0.230 |
.496 |
|
Ankle ROM (°) |
-0.014 |
.968 |
|
Hip ROM (°) |
0.060 |
.861 |
|
Note. Values represent Spearman's rank
correlation coefficients (ρ)
between ODI and primary outcomes (COP parameters and ROM). *p < .05, **p < .01 |
||
|
Variables |
p
(Spearman) |
p |
|
AP-range
(mm) |
0.014 |
.968 |
|
AP-velocity
(mm/s) |
0.271 |
.420 |
|
AP-RMS
(mm) |
-0.212 |
.532 |
|
ML-range
(mm) |
-0.515 |
.105 |
|
ML-velocity
(mm/s) |
-0.543 |
.085 |
|
ML-RMS
(mm) |
0.124 |
.716 |
|
Ankle
ROM (°) |
-0.253 |
.453 |
|
Hip
ROM (°) |
0.271 |
.420 |
|
Note.
Values represent Spearman's rank
correlation coefficients (ρ)
between ODI and primary outcomes (COP parameters and ROM). *p < .05, **p < .01 |
||
1. Primary outcomes
1) Changes in COP parameters
During stair ascent, significant reductions were observed in AP-range (p = .004, r = 0.86), AP-velocity (p = .006, r = 0.83), and ML-RMS (p = .021, r = 0.70). No significant changes were found in AP-RMS, ML-range, or ML-velocity. After Holm-Bonferroni correction, only AP-range (adjusted p = .024) and AP-velocity (adjusted p = .032) remained significant, while all ML-direction variables, including ML-RMS (p > .05), were no longer significant.
During stair descent, AP-range (p = .008, r = 0.80), AP-velocity (p = .016, r = 0.72), ML-range (p = .008, r = 0.80), ML-velocity (p = .033, r = 0.64), and ML-RMS (p = .003, r = 0.88) significantly decreased, while AP-RMS showed no significant change. After Holm-Bonferroni correction, AP-range (adjusted p = .024), AP-velocity (adjusted p = .032), and all ML parameters [ML-range (adjusted p = .016), ML-velocity (adjusted p = .033), ML-RMS (adjusted p = .009)] remained significant, whereas AP-RMS (p > .05) did not reach significance.
2) Changes in range of motion
During stair ascent, a significant increase was observed in ankle ROM (p = .006, r = 0.83), whereas no significant change was found in hip ROM. During stair descent, ankle ROM significantly decreased (p = .021, r = 0.70), while hip ROM showed no significant change.
2. Secondary outcomes
1) Changes in joint moment and walking speed
During stair ascent, a significant increase was observed in ankle moment (p = .003, r = 0.88), whereas no significant changes were found in hip moment. In addition, walking speed during stair ascent did not significantly change (p > .05).
2) Changes in ODI
The total ODI score significantly decreased from 12.45±4.32 at pre-intervention to 7.63±3.67 at post-intervention (t = 6.544, p = .001). The effect size (Cohen's d) was 1.97, indicating a very large change following the intervention.
3. Correlations of ODI with COP parameters and ROM
No significant correlations were found between ODI and the primary outcomes during stair ascent or descent.
This study aimed to analyze the effects of DNS training on stair gait performance, focusing on joint coordination and balance control, in middle-aged women with chronic low back pain. Chronic low back pain is generally accompanied by impaired neuromuscular control and postural instability, which can disrupt normal gait patterns and increase compensatory movement strategies during high-demand tasks such as stair climbing (Castro-Méndez et al., 2021; Koch and Hänsel, 2018, 2019). DNS training facilitates the activation of deep stabilizing muscles, thereby optimizing spinal segmental stability and body alignment, which enables efficient force transmission throughout the kinetic chain (Marchesi et al., 2024; Marinkovic et al., 2024). In this study, participants who underwent DNS training showed significant improvements in dynamic balance (COP), ankle joint range of motion and moment during stair ascent, as well as in the ODI. Additionally, ankle range of motion significantly decreased during stair descent, which may reflect either an adaptation prioritizing stability or a compen- satory adjustment. These findings suggest that DNS-based exercise may be associated with improvements in stair gait function in middle-aged women with chronic low back pain, while also indicating that adaptation patterns could vary depending on the task and direction.
The COP results in this study demonstrated selective rather than global improvements, depending on task and direction. During stair ascent in the AP family, both range and velocity remained significant after Holm correction, suggesting that forward movement of the center of gravity (COG) may have been achieved in a more efficient and controlled manner. Pro- pulsive force generation through the lower limbs and coord- ination between the trunk and lower extremities are essential during stair ascent to direct the COG forward (Hammond, Hatfield, Gilbart, Garland & Hunt, 2017; Lin, Fok, Schache & Pandy, 2015). DNS training may have contributed to these outcomes by enhancing anticipatory postural control in the forward direction through integrated regulation of respiration and deep stabilizing muscles, thereby potentially reducing excessive sway amplitude and velocity. This effect is consistent with findings from Lee et al. (2018), in which the DNS group demonstrated significantly shorter anticipatory control re- sponse times and greater improvements in balance regulation compared to a traditional core stabilization group, providing preliminary evidence that DNS may enhance central nervous system-based postural prediction mechanisms.
In contrast, ascent-ML RMS did not remain significant after correction, suggesting that improvements in mediolateral stability during ascent should be interpreted with caution. Although DNS training may have supported lateral stability during single-leg support, this effect was not statistically conclusive. Even so, the observed trend aligns with previous findings suggesting that DNS promotes joint centration, acti- vates deep stabilizers, and facilitates midline-directed weight shifts through dynamic positional transitions (Davidek, Andel & Kobesova, 2018; Kaushik & Ahmad, 2024). Such neuromuscular strategies contribute to more integrated trunk alignment and allow the COG to move along a trajectory closer to the GRF vector during movement. This result is also consistent with Kang, Park, and Ha (2024), who reported reductions in ML COP RMS after DNS training, reflecting enhanced trunk-centered stability and lateral control. Therefore, the reduction in ascent-ML RMS in this study should be regarded as exploratory evidence of DNS-related midline stabilization rather than as a definitive effect.
During stair descent, more consistent improvements were observed. In particular, the descent-ML family showed signifi- cant reductions in all three measures-range, normalized velocity, and RMS-even after Holm correction. This suggests that DNS training reduced excessive sway and reliance on compensatory strategies during single-leg landing, thereby strengthening mediolateral stability. Stair descent requires controlling down- ward acceleration and responding to substantial GRF at each step, necessitating active suppression of excessive COG motion (Grimmer, Zeiss, Weigand & Zhao, 2023; Stacoff, Diezi, Luder, Stüssi & Kramers-de Quervain, 2005). DNS training may have enhanced trunk stabilization and proprioceptive feedback during the load acceptance phase, thereby increasing the effi- ciency of deceleration and postural recovery (Marchesi et al., 2024; Marinkovic et al., 2024). These regulatory mechanisms may have contributed to reducing unnecessary mediolateral displacement of the center of gravity during stair gait and strengthening overall stability.
Collectively, DNS training demonstrated its most robust effects on forward propulsion control during ascent and on lateral stability during descent, while some outcomes remained at an exploratory level. These task- and direction-specific adap- tations support the interpretation that DNS training enhances anticipatory postural control, trunk-centered stability, and effi- cient weight transfer strategies, emphasizing its potential as an intervention to optimize dynamic balance under varying mechanical demands.
During stair ascent, participants showed a significant increase in ankle ROM, along with an increase in ankle joint moment at toe-off. This suggests a recovery of the propulsive function of the distal lower limb joint, likely supported by an improved moment arm at the ankle. In particular, the toe-off phase during stair ascent demands rapid plantarflexion of the ankle, which relies on effective neuromuscular coordination (Grimmer et al., 2023; Lin et al., 2015). The DNS training implemented in this study may have contributed to restoring the conditions necessary for efficient force production at the ankle joint by promoting joint centration, a principle that seeks to maintain the joint in its most biomechanically stable position (Kaushik & Ahmad, 2024; Mahdieh, Zolaktaf & Karimi, 2020). The observed increases in ROM and moment may suggest that more favorable conditions for ankle function were present. In contrast, hip ROM and moment did not show significant changes, with inconsistent tendencies observed-ROM de- creasing and moment increasing. These patterns should be interpreted cautiously as exploratory findings, which may reflect the high functional demands placed on the hip during stair ascent (Samuel, Rowe, Hood & Nicol, 2011) and the variability inherent to a small pilot sample. Future studies with larger cohorts are needed to clarify the role of hip contributions in relation to ankle function.
In this study, gait speed was examined as a complementary indicator, and no significant change was observed during stair ascent. Thus, the increase in ankle moment may not be solely attributable to gait speed. It could also be related to training-induced neuromuscular improvements, although this inter- pretation should be made with caution given the small sample size.
During stair descent, ankle ROM significantly decreased, while hip ROM showed a slight increasing trend. Stair descent is a task that requires the control of ground reaction forces and absorption of downward impact, and therefore demands a neuromuscular control strategy distinct from that used in ascent (Grimmer et al., 2023; Stacoff et al., 2005). The decrease in ankle ROM observed in this study may reflect an adaptation aimed at enhancing stability by limiting excessive distal motion, whereas the slight increase in hip ROM may indicate compen- satory involvement of proximal joints under high mechanical demand. These patterns are partially consistent with the core principle of DNS training-control from proximal to distal-suggesting that stabilization of the trunk and hip may have supported impact absorption and postural control during stair descent. However, these results should be interpreted with caution. Previous studies have shown that stair descent places considerable functional demands on the hip musculature (Foster, Maganaris, Reeves & Buckley, 2019; Samuel et al., 2011), and that when distal function is limited, proximal joints may act compensatorily to assist in controlling the center of mass (Moniz-Pereira, Kepple, Cabral, João & Veloso, 2018). Research in older adults has also suggested a distal-to-proximal redistribution of joint contributions, in which reduced ankle function may be offset by greater hip involvement (Browne & Franz, 2019; Delabastita et al., 2021). In light of these findings, the decrease in ankle ROM and the slight increase in hip ROM observed in this study may indicate the possibility of stabilization or redistribution processes. Nevertheless, given the small exploratory design, such interpretations should remain tentative, and further research with larger and more diverse cohorts is warranted to clarify their clinical significance in the context of DNS-based exercise.
In addition, the significant reduction in ODI following the DNS intervention may suggest the possibility of improved trunk and proximal control, which could be related to en- hanced functional capacity. Previous studies have shown that individuals with low back pain tend to rely excessively on distal strategies, particularly at the ankle, to compensate for impaired trunk stability, which can increase mechanical stress and exacerbate pain (van Dieën, Selen & Cholewicki, 2003; Shokouhyan et al., 2022). DNS training aims to restore trunk-centered stability (Frank et al., 2013; Kobesova & Kolar, 2014), thereby reducing the need for distal compensations and pro- moting more coordinated proximal control.
However, correlation analyses did not reveal direct asso- ciations between changes in ODI and changes in COP or ROM. This finding carries important implications. Self-reported dis- ability measures (e.g., ODI) and performance-based or bio- mechanical measures reflect different dimensions of function and are influenced by distinct patient characteristics, which may explain the lack of strong covariance between them (Wand, Chiffelle, O'Connell, McAuley & Desouza, 2010). More- over, previous research has shown that changes in movement patterns and changes in pain or activity limitation often do not occur simultaneously at the individual level, suggesting that symptom reduction and biomechanical adaptations may proceed along partially independent timelines (Wernli et al., 2020). Taken together, improvements in functional status (e.g., reduced disability) following interventions such as DNS may emerge through multiple pathways, including not only neuro- muscular retraining but also psychological and neurophysi- ological mechanisms, whereas COP and ROM primarily capture mechanical adaptations. Therefore, the absence of correlation between ODI and COP/ROM in the present study should not be interpreted as a lack of treatment effect, but rather as evidence of the multifactorial nature of recovery.
As such, the significance of this study may lie in the obser- vation that DNS training contributed to improvements in balance and ankle mobility, as reflected in the primary out- comes of COP and ROM, while the secondary outcome of joint moments provided additional support for enhanced co- ordination. In particular, the changes observed in ankle ROM and joint moments may not simply indicate variations in magnitude but rather suggest an adaptive redistribution of mechanical contributions between proximal and distal seg- ments, which appears to align with the core principles of DNS that emphasize trunk-centered stability and whole-body coordination. Moreover, the reduction in ODI can be regarded as supportive evidence of functional improvement; however, the absence of direct correlations with COP and ROM sug- gests that pain reduction and biomechanical adaptations may proceed independently. Overall, DNS training may not only contribute to improvements in specific biomechanical out- comes but also facilitate broader reorganization of motor control strategies, indicating its potential as a clinically mean- ingful approach for supporting stair gait recovery in middle-aged women with chronic low back pain.
This study has several limitations. First, it employed a single-group pre-post design without a control group, which limits the ability to attribute the observed improvements solely to the DNS intervention. Potential learning or placebo effects cannot be ruled out. Future studies should include comparison groups (e.g., usual care or core stabilization exercise) to strengthen causal inference. Second, as a pilot trial with a small sample size, the statistical power was limited, and the findings should be interpreted with caution. Larger randomized controlled trials are required to confirm these preliminary observations. Third, knee kinematics and kinetics were not included, despite the important role of the knee in stair negotiation. The analysis was focused on the redistribution of propulsive demand be- tween the ankle and hip joints. This omission should be con- sidered a limitation, and future studies should incorporate knee joint data to provide a more comprehensive biomechanical understanding. Fourth, the intervention period and follow-up were relatively short, and long-term adaptations remain unknown. Finally, the study population consisted only of middle-aged women with chronic low back pain, which may limit the generalizability of the findings to other groups. Future studies should include larger and more diverse cohorts, longer follow-up, and refined statistical approaches to confirm these preliminary results.
This pilot study investigated the effects of DNS training on stair gait function in middle-aged women with chronic low back pain. Following the DNS intervention, improvements were observed in balance control (COP), joint mobility, ankle joint moment, and the subjective functional index. These findings provide preliminary evidence that DNS may be associated with enhanced trunk stability and inter-joint coordination, thereby contributing to the harmony of lower limb joint function and the refinement of postural control strategies. While the results indicate preliminary potential benefits of DNS for stair gait performance and functional recovery in daily life, they should be interpreted with caution due to the small sample size and pilot nature of the study. Further confirmation in larger con- trolled trials is warranted.
References
1. Alshahrani, A., Reddy, R. S. & Ravi, S. K. (2025). Chronic low back pain and postural instability: Interaction effects of pain severity, age, BMI, and disability. Frontiers in Public Health, 13, 1497079.
Google Scholar
2. Babagoltabar-Samakoush, H., Aminikhah, B. & Bahiraei, S. (2025). Effectiveness of dynamic neuromuscular stabil- ization training on strength, endurance, and flexibility in adults with intellectual disabilities: A randomized con- trolled trial. Scientific Reports, 15(1), 768.
Google Scholar
3. Browne, M. G. & Franz, J. R. (2019). Ankle power biofeedback attenuates the distal-to-proximal redistribution in older adults. Gait & Posture, 71, 44-49.
Google Scholar
4. Buddhadev, H. H., Smiley, A. L. & Martin, P. E. (2020). Effects of age, speed, and step length on lower extremity net joint moments and powers during walking. Human Movement Science, 71, 102611.
Google Scholar
5. Castro-Méndez, A., Requelo-Rodríguez, I., Pabón-Carrasco, M., González-Elena, M. L., Ponce-Blandón, J. A. & Palomo-Toucedo, I. C. (2021). A case-control study of the effects of chronic low back pain in spatiotemporal gait parameters. Sensors (Basel), 21(15), 5247.
6. Chiu, S. L., Chang, C. C., Dennerlein, J. T. & Xu, X. (2015). Age-related differences in inter-joint coordination during stair walking transitions. Gait & Posture, 42(2), 152-157.
Google Scholar
7. Coulombe, B. J., Games, K. E., Neil, E. R. & Eberman, L. E. (2017). Core stability exercise versus general exercise for chronic low back pain. Journal of Athletic Training, 52(1), 71-72.
Google Scholar
8. Crenna, F., Rossi, G. B. & Berardengo, M. (2021). Filtering bio- mechanical signals in movement analysis. Sensors, 21(13), 4580.
Google Scholar
9. Davidek, P., Andel, R. & Kobesova, A. (2018). Influence of dynamic neuromuscular stabilization approach on max- imum kayak paddling force. Journal of Human Kinetics, 61, 15-27.
Google Scholar
10. de Sousa, C. S., de Jesus, F. L. A., Machado, M. B., Ferreira, G., Ayres, I. G. T., de Aquino, L. M., Fukuda, T. Y. & Gomes-Neto, M. (2019). Lower limb muscle strength in patients with low back pain: A systematic review and meta-analysis. Journal of Musculoskeletal & Neuronal Interactions, 19(1), 69-78.
Google Scholar
11. Delabastita, T., Hollville, E., Catteau, A., Cortvriendt, P., De Groote, F. & Vanwanseele, B. (2021). Distal-to-proximal joint mechanics redistribution is a main contributor to reduced walking economy in older adults. Scandinavian Journal of Medicine & Science in Sports, 31(5), 1036-1047.
Google Scholar
12. Firouzabadi, A., Arjmand, N., Zhang, T., Pumberger, M. & Schmidt, H. (2024). Effect of low back pain on the kinetics and kinematics of the lumbar spine – A combined in vivo and in silico investigation. Journal of Biomechanics, 164, 111954.
Google Scholar
13. Foster, R. J., Maganaris, C. N., Reeves, N. D. & Buckley, J. G. (2019). Centre of mass control is reduced in older people when descending stairs at an increased riser height. Gait & Posture, 73, 305-314.
Google Scholar
14. Frank, C., Kobesova, A. & Kolar, P. (2013). Dynamic neuro- muscular stabilization & sports rehabilitation. International Journal of Sports Physical Therapy, 8(1), 62-73.
Google Scholar
15. Gibbs, D., McGahan, B. G., Ropper, A. E. & Xu, D. S. (2023). Back pain: Differential diagnosis and management. Neurologic Clinics, 41(1), 61-76.
Google Scholar
16. Goldberg, S. R. & Stanhope, S. J. (2013). Sensitivity of joint moments to changes in walking speed and body-weight-support are interdependent and vary across joints. Journal of Biomechanics, 46(6), 1176-1183.
Google Scholar
17. Gorji, S. M., Mohammadi Nia Samakosh, H., Watt, P., Henrique Marchetti, P. & Oliveira, R. (2022). Pain neuroscience edu- cation and motor control exercises versus core stability exercises on pain, disability, and balance in women with chronic low back pain. International Journal of Environ- mental Research and Public Health, 19(5), 2694.
Google Scholar
18. Grimmer, M., Zeiss, J., Weigand, F. & Zhao, G. (2023). Joint power, joint work and lower limb muscle activity for transitions between level walking and stair ambulation at three inclinations. PLoS ONE, 18(11), e0294161.
Google Scholar
19. Hammond, C. A., Hatfield, G. L., Gilbart, M. K., Garland, S. J. & Hunt, M. A. (2017). Trunk and lower limb biomech- anics during stair climbing in people with and without symptomatic femoroacetabular impingement. Clinical Bio- mechanics, 42, 108-114.
Google Scholar
20. Huang, H., Xie, H., Zhang, G., Xiao, W., Ge, L., Chen, S., Zeng, Y., Wang, C. & Li, H. (2025). Effects of dynamic neuro- muscular stabilization training on the core muscle con- tractility and standing postural control in patients with chronic low back pain: A randomized controlled trial. BMC Musculoskeletal Disorders, 26(1), 213.
Google Scholar
21. Kang, S., Park, I. & Ha, M. S. (2024). Effect of dynamic neuro- muscular stabilization training using the inertial load of water on functional movement and postural sway in middle-aged women: A randomized controlled trial. BMC Women's Health, 24(1), 154.
Google Scholar
22. Kaushik, M. & Ahmad, I. (2024). Bridging dynamic neuro- muscular stabilization synergism with movement control impairment related non-specific low back pain: Scoping review. Journal of Musculoskeletal and Neuronal Inter- actions, 24(4), 420-432.
Google Scholar
23. Khowailed, I. A. & Lee, H. (2021). Neuromuscular control of ankle-stabilizing muscles: Specific effects of sex and men- strual cycle. International Journal of Sports Medicine, 42(3), 270-276.
Google Scholar
24. Kienbacher, T., Fehrmann, E., Habenicht, R., Koller, D., Oeffel, C., Kollmitzer, J., Mair, P. & Ebenbichler, G. (2016). Age- and gender-related neuromuscular pattern during trunk flexion-extension in chronic low back pain patients. Journal of Neuroengineering and Rehabilitation, 13, Article 16.
Google Scholar
25. Kobesova, A. & Kolar, P. (2014). Developmental kinesiology: Three levels of motor control in the assessment and treatment of the motor system. Journal of Bodywork and Movement Therapies, 18(1), 23-33.
Google Scholar
26. Koch, C. & Hänsel, F. (2018). Chronic non-specific low back pain and motor control during gait. Frontiers in Psychology, 9, 2236.
Google Scholar
27. Koch, C. & Hänsel, F. (2019). Non-specific low back pain and postural control during quiet standing—A systematic review. Frontiers in Psychology, 10, 586.
Google Scholar
28. Kofotolis, N., Kellis, E., Vlachopoulos, S. P., Gouitas, I. & Theodorakis, Y. (2016). Effects of Pilates and trunk streng- thening exercises on health-related quality of life in women with chronic low back pain. Journal of Back and Musculoskeletal Rehabilitation, 29(4), 649-659.
Google Scholar
29. Kovacikova, Z., Sarvestan, J., Neumannova, K., Linduska, P., Gonosova, Z. & Pecho, J. (2020). Balance control during stair descent on compliant surface is associated with knee flexor and ankle plantar flexor strength in older adults. Journal of Biomechanics, 111, 110013.
Google Scholar
30. Kuai, S., Guan, X., Zhou, W., Zhang, R., Ji, R., Liao, Z., Guo, D., Liu, W. & Wang, D. (2018). Continuous lumbar spine rhythms during level walking, stair climbing and trunk flexion in people with and without lumbar disc herniation. Gait & Posture, 63, 296-301.
Google Scholar
31. Lee, N. G., You, J. S. H., Yi, C. H., Jeon, H. S., Choi, B. S., Lee, D. R., Park, J. M., Lee, T. H., Ryu, I. T. & Yoon, H. S. (2018). Best core stabilization for anticipatory postural adjustment and falls in hemiparetic stroke. Archives of Physical Medicine and Rehabilitation, 99(11), 2168-2174.
Google Scholar
32. Lin, Y. C., Fok, L. A., Schache, A. G. & Pandy, M. G. (2015). Muscle coordination of support, progression and balance during stair ambulation. Journal of Biomechanics, 48(2), 340-347.
Google Scholar
33. Lima, M., Ferreira, A. S., Reis, F. J. J., Paes, V. & Meziat-Filho, N. (2018). Chronic low back pain and back muscle activity during functional tasks. Gait & Posture, 61, 250-256.
Google Scholar
34. Mahdieh, L., Zolaktaf, V. & Karimi, M. T. (2020). Effects of dynamic neuromuscular stabilization (DNS) training on functional movements. Human Movement Science, 70, 102568.
Google Scholar
35. Maher, C., Underwood, M. & Buchbinder, R. (2017). Non-specific low back pain. The Lancet, 389(10070), 736-747.
Google Scholar
36. Marchesi, G., Arena, G., Parey, A., De Luca, A., Casadio, M., Pierella, C. & Squeri, V. (2024). A strong core for a strong recovery: A scoping review of methods to improve trunk control and core stability of people with different neuro- logical conditions. Applied Sciences, 14(11), 4889.
Google Scholar
37. Marinkovic, D., Macak, D., Stanic, V., Madic, D. M., Radanovic, D., Gojkovic, Z., Spasic, M., Ilic, A., Trivic, T. & Drid, P. (2024). Effect of different neuromuscular training modalities on postural stability in healthy recreation people: A random- ized controlled trial. Scientific Reports, 14, 32097.
Google Scholar
38. McFadyen, B. J. & Winter, D. A. (1988). An integrated bio- mechanical analysis of normal stair ascent and descent. Journal of Biomechanics, 21(9), 733-744.
Google Scholar
39. Meucci, R. D., Fassa, A. G. & Faria, N. M. (2015). Prevalence of chronic low back pain: Systematic review. Revista de Saúde Pública, 49, Article 1.
Google Scholar
40. Moniz-Pereira, V., Kepple, T. M., Cabral, S., João, F. & Veloso, A. P. (2018). Joint moments' contributions to vertically accelerate the center of mass during stair ambulation in the elderly: An induced acceleration approach. Journal of Biomechanics, 79, 105-111.
Google Scholar
41. Perrin, T. P., Morio, C. Y. M., Besson, T., Kerhervé, H. A., Millet, G. Y. & Rossi, J. (2023). Comparison of skin and shoe marker placement on metatarsophalangeal joint kinematics and kinetics during running. Journal of Biomechanics, 146, 111410.
Google Scholar
42. Pizol, G. Z., Miyamoto, G. C. & Cabral, C. M. N. (2024). Hip biomechanics in patients with low back pain: What do we know? A systematic review. BMC Musculoskeletal Disorders, 25(1), 415.
Google Scholar
43. Poulsen, K. M. & Cabell, L. (2024). Surface electromyography and kinetics during step descent in individuals with low-level chronic or recurrent low back pain and lumbar instability. Journal of Orthopaedics, Trauma and Rehabili- tation, 31(1), 21-27.
Google Scholar
44. Samuel, D., Rowe, P., Hood, V. & Nicol, A. (2011). The bio- mechanical functional demand placed on knee and hip muscles of older adults during stair ascent and descent. Gait Posture, 34(2), 239-244.
Google Scholar
45. Shokouhyan, S. M., Davoudi, M., Hoviattalab, M., Abedi, M., Bervis, S., Parnianpour, M., Brumagne, S. & Khalaf, K. (2022). Distinction of non-specific low back pain patients with proprioceptive disorders from healthy individuals by linear discriminant analysis. Frontiers in Bioengineering and Biotechnology, 10, 1078805.
Google Scholar
46. Stacoff, A., Diezi, C., Luder, G., Stüssi, E. & Kramers-de Quervain, I. A. (2005). Ground reaction forces on stairs: Effects of stair inclination and age. Gait & Posture, 21(1), 24-38.
Google Scholar
47. Steingrebe, H., Sell, S., Ehmann, H. & Stein, T. (2025). Hip and trunk biomechanics and dynamic balance during steady-state stair walking in people with mild-to-moderate hip osteoarthritis. Journal of Biomechanics, 185, 112709.
Google Scholar
48. Stöwhas, K., Droppelmann, G., Jorquera, C. & Feijoo, F. (2024). Postural and lumbopelvic control: Crucial factors in the functionality of patients with low back pain—A descriptive cross-sectional study. Journal of Clinical Medicine, 13(13), 3836.
Google Scholar
49. Sung, W., Abraham, M., Plastaras, C. & Silfies, S. P. (2015). Trunk motor control deficits in acute and subacute low back pain are not associated with pain or fear of movement. The Spine Journal, 15(8), 1772-1782.
Google Scholar
50. Tong, M. H., Mousavi, S. J., Kiers, H., Ferreira, P., Refshauge, K. & van Dieën, J. (2017). Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Archives of Physical Medicine and Rehabilitation, 98(1), 120-136.e2.
Google Scholar
51. van Dieën, J. H., Selen, L. P. & Cholewicki, J. (2003). Trunk muscle activation in low-back pain patients: An analysis of the literature. Journal of Electromyography and Kinesiology, 13(4), 333-351.
Google Scholar
52. Victora Ruas, C. & Vieira, A. (2017). Do muscle strength imbalances and low flexibility levels lead to low back pain? A brief review. Journal of Functional Morphology and Kinesiology, 2(3), 29.
Google Scholar
53. Violante, F. S., Mattioli, S. & Bonfiglioli, R. (2015). Low-back pain. Handbook of Clinical Neurology, 131, 397-410.
54. Vlaeyen, J. W. S., Maher, C. G., Wiech, K., Van Zundert, J., Meloto, C. B., Diatchenko, L., Battié, M. C., Goossens, M., Koes, B. & Linton, S. J. (2018). Low back pain. Nature Reviews Disease Primers, 4(1), 52.
55. Wand, B. M., Chiffelle, L. A., O'Connell, N. E., McAuley, J. H. & Desouza, L. H. (2010). Self-reported assessment of dis- ability and performance-based assessment of disability are influenced by different patient characteristics in acute low back pain. European Spine Journal, 19(4), 633-640.
Google Scholar
56. Wenzel, T. A., Hunt, N. L., Holcomb, A. E., Fitzpatrick, C. K. & Brown, T. N. (2023). Surface, but not age, impacts lower limb joint work during walking and stair ascent. Journal of Functional Morphology and Kinesiology, 8(4), 145.
Google Scholar
57. Wernli, K., Tan, J. S., O'Sullivan, P., Smith, A., Campbell, A. & Kent, P. (2020). Does movement change when low back pain changes? A systematic review. Journal of Orthopaedic & Sports Physical Therapy, 50(12), 664-670.
Google Scholar
58. Wohlgemuth, K. J., Arieta, L. R., Brewer, G. J., Hoselton, A. L., Gould, L. M. & Smith-Ryan, A. E. (2021). Sex differences and considerations for female-specific nutritional strategies: A narrative review. Journal of the International Society of Sports Nutrition, 18(1), 27.
Google Scholar
59. Yoon, H. S. & You, J. S. H. (2017). Reflex-mediated dynamic neuromuscular stabilization in stroke patients: EMG pro- cessing and ultrasound imaging. Technology and Health Care, 25(S1), 99-106.
Google Scholar
60. Zahedi, H. & Kiyani, R. (2020). Comparing the effects of core stability and Williams training on dynamic balance and back pain in women with chronic back pain. Sport Sciences and Health Research, 12(1), 101-112.
Google Scholar